 |
BRIEFING - October 2003
En Français
The health service brain drain -- what are the options for change?
Every year, health workers leave low-income countries in the thousands to seek better pay and professional prospects abroad. Rather than try to prevent the free movement of people, countries and their international partners are now seeking workable and ethical solutions
DR FRANK Nyonator has a major problem. As director of policy and planning for Ghana’s health service, he is losing a stream of nurses, doctors and pharmacists abroad every year. “With the nurses, we are talking in terms of thousands,” he says. Most head for the United States and the United Kingdom for higher pay and better education prospects; few return. Not only does their departure leave holes in an overstretched health system; it also deprives Ghana of the return on investment in their training, and effectively subsidies the health systems of much richer countries that have failed to “grow their own” workers in adequate numbers.
Ghana is not, of course, unique. The health workers’ brain drain is also damaging other developing countries, particularly in Africa. Among those worst affected are South Africa, Zimbabwe and Nigeria. In some of these countries, the rate at which nurses are lost appears to be accelerating. While industrialized countries such as the US and the UK have long filled the gaps in their nursing workforces from abroad, they have traditionally relied on countries that have trained more nurses than they need - such as the Philippines. Today the rich countries are increasingly employing nurses not only from the traditional “exporting” countries but also from African countries that have acute staffing shortages of their own. There is no one to fill the posts that their emigrant workers vacate, and health services - their immunization programmes included - are suffering.
Dr Nyonator understands exactly why health workers want to leave lowincome countries. “The reasons are not secret,” he says. First, the pay is poor and may not stretch to buy such luxuries as a house or a car. “People are scared that, if they remain in the system, they will not be able to make ends meet. Pension schemes are not adequate and people just want to make sure that they have got something that will provide them with security in the future.” Second, says Dr Nyonator, among doctors and pharmacists, there is a demand for postgraduate training, which until now has not been widely available from domestic institutions. The limited postgraduate facilities that exist have been dysfunctional, he says.
Measuring the flow of staff
Accurate information on the scale of the “human resources” shortage is difficult to find. There are no comprehensive databases. But the patchy available figures hint at serious annual losses from countries that can ill afford to lose any health workers. Around 2500 nurses applied to emigrate from South Africa in 2001 (1). The Ghana Registered Nurses’ Association says that more than 3000 nurses left the country in 2003. In 2001, 473 nurses from Zimbabwe registered to work in the UK alone. That might sound like a small number, until you discover that the total number of nurses to qualify in Zimbabwe that year was only 737. Other African countries with a small cadre of nurses, such as Malawi, are also seeing sharp increases in the numbers lost, largely to the UK (Figure 1). Physicians are also leaving lowincome countries in large numbers, although their numbers do not appear to be rising like those of nurse emigrants. In the US, 30% of migrant physicians are from India and Pakistan and in the UK, 20% of migrant physicians are from Africa.
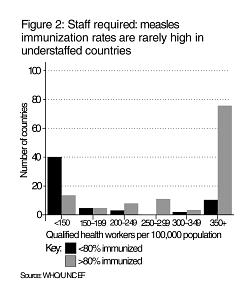 |
The outward flow of staff is not matched by equal numbers coming in to these countries, so vacancies in nursing and specialist medical positions are widespread. For example, in South Africa, 60% of institutions surveyed said that they had trouble recruiting staff to replace emigrants (1), while Malawi reported that almost 53% of nursing posts were vacant in 1998 (2). Inevitably, this causes problems in delivering healthcare; for example, measles immunization coverage tends to be high when staffing ratios are good, and low when staffing ratios are poor (Figure 2).
One particular problem is the loss of specialist staff with years of experience; their numbers are small, but the holes that they leave may take as many years again to fill. Adelaide Shearley is WHO advisor for the Expanded Programme on Immunization in Namibia, and has also worked for the immunization programmes of two additional countries in sub-Saharan Africa. In each, she has watched colleagues leave specialist roles in public health - such as surveillance - to take up more general clinical nursing posts abroad. “All the investment is lost,” she says.
Wake-up calls
Not before time, the brain drain in health workers is attracting new attention - from governments and from international players such as WHO, the OECD and the Rockefeller Foundation. The GAVI partners have also recognized that the shortage of health workers must be addressed if countries are to meet their targets for increasing immunization coverage within a sustainable health system. WHO, which has set up a programme of work on human resources, is currently gathering much-needed data on health workers’ migration before considering the possible policy options for governments. But, warns Dr Barbara Stilwell at WHO, there will be no quick fix: “It’s not as simple as some people would like to think.”
Indeed, many simplistic responses have been proposed. “People zoom in with knee-jerk reactions,” says Dr Akram Eltom at the International Organization for Migration. “For example, they suggest raising the cost of emigration, or raising other barriers [to emigrants].” But, he says, it would be unethical to prevent workers from leaving their country of origin. Indeed, globalization has positively encouraged an international market for skills in numerous other areas, such as information technology. Why, then, should healthcare skills be viewed differently?
People have a right to move, to seek improved career prospects and secure incomes. Poor working conditions, a lack of education opportunities and low pay act as “push” factors in poor countries, while the “pull” factors in richer countries include the promise of wages up to 25 times higher than at home, safer working conditions, and better opportunities for continuing professional development, says Dr Stilwell. Equally important, health workers who emigrate continue to contribute to the economies of their country of origin, because of the money they send home to their families. In fact, money sent home by emigrant workers to their families in developing countries now exceeds the total official development assistance paid by governments in industrialized countries, says Dr Stilwell. The money is not ploughed back into a health service, however.
Ways to change
In the search for intelligent responses to the problem, analysts are now looking in greater depth at the reasons why health workers leave their home countries, with the aim of informing new policies and identifying ways to change behaviour.
Dr Marko Vujicic, an economist, and his colleagues at WHO have assessed the importance of salary in attracting health workers from developing to industrialized countries. Their conclusion, says Vujicic, is that salaries are a key factor influencing the supply of migrants, although not the only important factor. The differences in earnings between richer and poorer countries are stark, even when the figures are adjusted for purchasing power to take account of differences in the cost of living between countries. For example, says Vujicic, the nurse wage in Australia and Canada is about 25 times the nurse wage in Zambia, about 14 times the nurse wage in Ghana and about twice the nurse wage in South Africa. For doctors, the differences are similarly large.
But other factors, such as living conditions, safety at work and the options for professional development also seem to be important. If wages were the only factor, says Vujicic, the countries whose workers stand to gain the largest income increase from leaving should in theory have the highest numbers of would-be emigrants. In this case, for example, Ghanaian nurses should be keener to leave home than South African nurses, because South African nurses can “only” double their earnings while Ghanaians can increase theirs 14 times. In reality, the proportion of health workers who intend to emigrate from South Africa is approximately equal to that in Ghana, suggesting that other factors beyond money influence workers’ decisions.
Staff motivation is clearly important too, says Dr Stilwell. Motivation matters in any workplace, but where rising numbers of staff are leaving, it can rapidly deteriorate. Moving abroad can symbolise optimism about one’s working future, while staff left behind can become demoralised. This is most likely when supervision is inadequate, workloads are heavy, and managers have little authority to demand more time from people who are earning a pittance in poor working conditions.
Ethical responses
Governments in low-income countries are beginning to discuss ways to increase their health worker’s incentives to stay. Options include better housing, transport to work, cheap car loans and even basic occupational health improvements to make nurses’ work safer. For example, Dr Nyonator says, proposals currently being considered by the government of Ghana include favourable car loans, housing loan schemes, and increased remuneration for staff willing to work in remote rural areas. The government is also setting up a postgraduate medical college, which is due to begin training in 2004.
Industrialized countries’ responsibilitieS
Increasingly, however, analysts agree that the problem cannot be solved by the low-income countries alone. The International Council of Nurses, which with WHO and others has recently analysed the international flow of staff (1), says that it is unacceptable for rich countries with “dysfunctional” health systems, characterised by an inability to “grow their own and keep their own” staff, to exploit the push factors in the developing countries from which they recruit their much-needed staff.
Aggressive recruitment of nurses from developing countries may give the rich countries a quick fix, says the ICN, but it will not produce lasting solutions to their domestic problems. Rather, the countries with the worst staffing shortages - such as the UK - should assess the reasons for their failure to recruit and retain their own workers and change their own policies.
Governments in industrialized countries are now being asked to consider various other options. For example, international development assistance funds, which would not normally be spent on staff costs, could be used to boost some aspects of the remuneration package for health workers who stay in their own countries. Governments in industrialized countries that poach workers from developing countries might be required to pay compensation to the source country for the costs of each worker’s training and also, possibly, the loss of tax revenue.
Athough such schemes may sound relatively radical, Ghana is just one country that has already discussed with partners such as the World Bank ways to use international development money to boost the remuneration packages of health workers. “There has been a good response,” says Dr Nyonator. Perhaps, at last, there is a prospect of change.
Phyllida Brown
References
(1) International nurse mobility: trends and policy implications. (2003). International Council of Nurses/WHO/Royal College of Nursing. Geneva. www.icn.ch
(2) Developing evidence-based ethical policies on the migration of health workers: conceptual and practical challenges. (2003). Stilwell. B. et al. Human Resources for Health, in press.
(3) Dovlo, D., Nyonator, F. Migration by Graduates of the University of Ghana Medical School: A preliminary rapid appraisal. Human Resources for Health Development Journal. Jan-April 1999. 3 : 40-51.
Immunization Focus October 2003 - Contents
 |
 |