| |

March 2001
Return to March
2001 contents page
SPECIAL FEATURE
First, do no harm
Lisa Jacobs examines the road to
injection safety – from recognition of the problem to action
YOU may already know: unsafe injection
practices spread disease. In a tragic twist of irony, health workers
who aim to improve people’s health may be unintentionally spreading
harm with every prick of an unsterile needle, every time they toss
a used disposable syringe in a vat of warm water for eventual re-use,
or drop it in a trash can.
|
The result? From 8 million to 16
million new hepatitis B infections, 2.3 million to 4.7 million
new hepatitis C infections and 80,000 to 160,000 new HIV infections
every year. These chronic infections are responsible for an
estimated 1.3 million early deaths and lead to US$ 535 million
in direct medical costs every year.
Injections are prescribed for
a wide variety of reasons. While they are essential for delivery
of vaccines and many treatments, they are also given for other,
questionable reasons. The belief that an injection is the
most powerful and quick way to deliver medicine – even
if the syringe contains nothing but vitamins – contributes
to over-demand for, and over-prescribing of, injections. In
fact, the majority of injections given for curative reasons
in developing countries are thought to be unnecessary.
|
|
|
| |
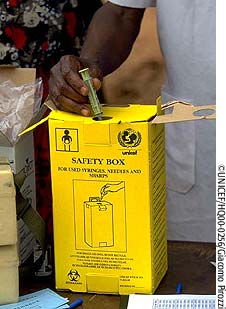
Look what I’ve found:
children playing with discarded syringes
|
Why are unsafe injections tolerated –
by health workers, patients, caretakers, government officials? The
answers are complex and include economic imperatives and cultural
attitudes about waste. But perhaps the most important reason is
that the people with decision-making power – including patients
and caretakers of children – do not understand the risks, the
extent of the problem, or that solutions (Box 1) are well within
reach.
According to Dr Yvan Hutin, an epidemiologist
and hepatitis B expert who runs the Safe Injection Global Network
(SIGN), understanding the problem is the first and most crucial
step.
In fact, in many cases, as soon as people
see the evidence of what is occurring, they are convinced they must
do something about it, says Dr Hutin. "The problem of unsafe injections
will not solve itself. But when safety is included in health sector
plans and budgets, it will improve."
A problem with clear solutions
In 1995, a study in Burkina Faso
found that only one in ten injections in rural health centres was
performed with sterile equipment. A new system was then introduced
that made essential drugs – including disposable, sterile syringes
– readily available at every health centre through a cost recovery
scheme. Five years later, the impact on safety was astounding: by
2000 nearly 100% of injections in the centres surveyed were given
with a sterile syringe. In this instance, increased supply of syringes
led to increased demand – a demand for which people were willing
to pay.
"The Burkina Faso experience shows
how incredibly amendable this problem is," said Dr Hutin. "Sometimes
it is just a matter of making clean needles available."
The supply, or logistics, approach that
worked in Burkina Faso will not be the answer for all countries.
Demand led to supply in Romania, where a highly publicised outbreak
of HIV infections occurred among orphans in the early nineties.
Children had been infected through blood transfusions and injections
conducted in orphanages.
With the vivid images of medically-induced
HIV infection, concern about contracting diseases from syringes
built among the general public. People demanded new syringes, in
sealed packages, for every injection, and the system responded.
"Every time an intervention has
been funded and attempted, regardless as to whether it was behaviour
change, provision of supplies or sharps waste management, it showed
some impact," says Dr Hutin. "So if we have a sector wide approach
that combines all these low-cost interventions, we should be able
to eliminate unsafe injection practices."
EPI: a small part of the problem,
a big part of the solution
Even though immunization injections
account for fewer than 10% of the 12 billion injections given annually,
most health systems have considered injection safety the responsiblity
of the immunization programme, or EPI. Unfortunately, that responsibility
has not been supported with appropriate budgets. And even though
it is essential that immunization programmes have safe practices,
EPI managers have no control over the use and over-use of injections
in the greater health system.
"We can’t solve the problem,"
says Dr Caroline Akim, EPI Manager in Tanzania. "But we can act
as advocates, and push the health system to address it." In fact,
advocating for safe injection policies and practices is an opportunity
for immunization programmes to have a profound, system-wide impact.
The first priority, according to many,
is to adopt a policy on safe injection and disposal. "Having a system-wide
policy is necessary to extend responsibility for injection safety
to the whole health sector, instead of just in EPI," says Dr Akim.
A national policy also gives programmes the authority to seek out
and put an end to actions that are unsafe.
However, a policy is only as good as
its implementation. Without buy-in by all stakeholders, a safe injection
and disposal policy will just be another rule on the books –
one that may be considered a nuisance, adding costs to programmes
and perhaps even depriving people of much needed income.
"A policy that is not followed
is just like having no policy at all," said Dr. B. Wabudeya, Minister
of State for Health in Uganda. And the
danger is that those in roles of responsibility may think that once
a policy is drafted and adopted, the situation has been addressed.
Measuring the problem
If discovery is the first step
toward solving the problem, the first step has just been made easier.
A simple, focused methodology for tracking injection and disposal
practices, and documenting knowledge and understanding among health
workers and patients, has just been developed jointly by SIGN, the
World Health Organization and BASICS, a programme funded by the
US Agency for International Development. Referred to as ’Tool
C’ (as in, third of a series of four), this new methodology
has been tested in Burkina Faso, Niger, Ethiopia, Mali, Mauritania,
Zimbabwe and Egypt(1). The aim is to make it as easy for governments
to monitor injection safety as to monitor the percentage of all
children immunized, or coverage. "What is the good of increasing
coverage if you also increase exposure to hepatitis B and C, or
HIV?" asks Hutin.
The methods behind Tool C are simple.
In each country, a team of 12 monitors activities in 80 health centres
in 10 districts over 2 weeks. Importantly, the data collected are
practical, so countries can quickly identify solutions. For example,
the team finds out how many health centres have dedicated areas
for the preparation of injections, and whether they have at least
a week’s supply of disposable/AD equipment in stock. The measures
are standardized, so, as more countries undertake the process, common
problems can be highlighted and appropriate actions designed.
Dangerous waste
Tool C identified a serious problem
in Burkina Faso, one that has caught many communities unprepared.
Investigators found needles discarded in open containers in 66 health
centres, putting health workers at risk of accidental needle-stick
injuries. At most of the centres, used needles and syringes were
found in the surrounding environment, putting the larger community
at risk – a situation that has been identified in a number
of countries.
"In many developing countries,
collection and removal of waste is considered to be a municipal
responsibility – not that of the hospitals and health system,"
says Annette Prüss, from the environmental safety division
at WHO. "The concept of ’polluter pays’ is a very Western
concept."
Not only do children find syringes to
be effective squirt toys; in many countries, scavengers also scour
refuse for saleable items. Conventional disposable syringes can
be rinsed, re-packaged and re-sold as new, when they are not in
fact sterile. According to environmental experts, some health workers
actually collect used syringes to sell to recyclers, providing income
for both. And risk for many.
Now, having learned of their waste disposal
problem, health officials in Burkina Faso have developed plans to
address it. Their chances for success are high; a recent assessment
in Côte d’Ivoire found that facilities which took responsibility
for healthcare waste as part of their duty of care successfully
eliminated dirty sharps from their environment.
"What is needed above all is the
will to take care of the problem," says Dr Hutin.
Technology to the rescue?
Many countries are addressing injection
safety by making the switch to AD syringes for immunizations. AD
syringes have a mechanism designed to lock the syringe once it is
used, so that it cannot be re-used. Countries that have been approved
to receive vaccines from GAVI and the Vaccine Fund will also receive
the requisite number of AD syringes. GAVI is now weighing a policy
to further help countries with the transition from sterilizable
and/or disposable syringes to AD syringes for all vaccines, in order
to support countries to comply with the policy of WHO, UNICEF and
UNFPA to use AD syringes for all immunizations by 2003.
|
But when it comes to safety, technology
is not the entire solution. "If you want to learn how to re-use
an ’auto-disable’ syringe, come to Pakistan," says
Johnny Thaneoke Kyaw-Myint, Senior Project Officer for Health
and Nutrition with UNICEF Pakistan. He was, of course, not
serious. "People have learned how to manipulate the syringe
so that the safety mechanism doesn’t catch. So it can
be re-used, or sold and re-used, again."
The lesson? People must be educated,
motivated and supported to insist upon a sterile syringe with
every injection. Provision of safe injection equipment should
be part of a broader strategy that also includes encouraging
behaviour change and the management of sharps waste.
At present, 500 million AD syringes
are produced annually for use in developing countries. Within
two years, as more and more countries follow, that number
is expected to rise to 2 billion. The disposal issue becomes
more critical each day.
Simple actions can be taken immediately,
says Dr Prüss. Supplies of sharps boxes should be available
in all health centres – not just in time for immunization
campaigns. Small incinerators can be built; local oven-builders
can be employed to build incinerators. The costs are affordable;
a small incinerator to serve a district can be built for under
US$700, according to Dr John Lloyd, an immunization expert
with the Bill and Melinda Gates Children’s Vaccine Program
at PATH.
|
|
 |
| |
A good start: safety boxes
reduce the risks but their final disposal must be safe too |
Until recently, the problem of unsafe
injections seemed insurmountable, says Dr Hutin. "But in fact, when
one looks at the experience acquired, we now know that safety is
an area that is easy to address – if the health system decides
to address it. We know some simple strategies to follow, and results
are visible and quick."
Reference
(1) Full series
and available summary results at: http://www.injectionsafety.org/html/resources.html
|
Country file 1: Pakistan –
a country ready for change
SOME would be daunted by
the scale of the challenges facing Pakistan’s newly formed
injection safety network. But Dr Arshad Altaf, one of the
key organisers of the network, does not sound like the daunted
type.
"There are no short cuts;
we need education and training, and we need injection safety
to get the attention and priority that it deserves," says
Dr Altaf, a medical doctor and behavioural epidemiologist
from the Aga Khan University in Karachi.
The burden of bloodborne infections
in Pakistan is heavy. As many as one in ten of the general
population is a chronic carrier for hepatitis B virus (HBV).
And, in the past few years, hepatitis C virus (HCV) has spread
rapidly; in some parts of Pakistan, more than one in 20 people
are chronic carriers. Researchers have concluded that unsafe
injections are the most likely cause of this growing HCV epidemic.
And since HCV is even more likely than HBV to cause chronic
liver disease, the burden of long-term illness is rising.
Unnecessary injections
Studies in Hafizabad, southwest
of Lahore, and Darsano Channo, near Karachi, both found that
exposure to injections was the strongest risk factor for being
infected with hepatitis; the more injections, the greater
the probability of being infected(1).
"Painkillers, antibiotics,
antimalarials, steroids and multivitamins are all given by
injection," says Dr Altaf. All at a price: patients often
pay 30 Pakistan rupees (about US $0.50) for an injection when
the whole household’s income is often as low as US$1.60
a day. "When the supply of syringes runs out, the clinics
just dip the syringe in water and re-use it," says Dr Altaf.
In a study at Aga Khan University
Hospital, Dr Naheed Nabi and others(2)
found that most patients believed injections were more effective
than oral medications, and were willing to pay more for them.
But when told that oral medications are equally effective,
four-fifths of patients said they would prefer to avoid an
injection.
Interestingly, 91 per cent of
the patients who received injectable treatments said that
their doctors recommended them, disputing the claim that health
workers are merely responding to demand. Only 9 per cent of
patients had requested injections.
Recycled syringes
A further problem is waste
disposal. "There is no proper management or disposal system
for waste," says Dr Altaf. His team have tracked the final
destinations of syringes from hospitals and clinical laboratories
in Karachi. Many are dumped at community waste sites where
scavenger boys collect them and sell them to dealers. Some
are also sold to scavengers by cleaners at the clinics and
labs.
"The used syringes with
needles are sold by the kilogram at up to 10 Pakistan rupees
[17 US cents]," says Dr Altaf. Needles are removed by the
dealers and are re-moulded. The syringe plastic is washed,
crushed and made into granules, which are sold on to the plastic
ware industry. A minority of syringes are also repackaged
and sold for repeat medical use.
The earnings
from the hazardous trade of recycling used syringes might
seem small to comfortable outsiders sitting in the industrialized
countries. But to people on low incomes, they are significant,
says Dr Altaf. "With the financial incentive and the culture
of re-use being so ingrained in the country, we expect that
recycling will continue," he says.
Educate the scavengers
Pakistan must develop a
proper system(3) for clinical waste
disposal, Dr Altaf believes. This, together with the eventual
use of autodisable (AD) syringes in the country’s immunization
clinics, may reduce the risks of bloodborne infections. But
until doctors and patients gain a greater understanding of
the risks of infection, and the number of unnecessary therapeutic
injections falls, large numbers of conventional disposable
syringes will continue to enter community waste dumps. Dr
Altaf believes that it may be pragmatic to educate those involved
in the recycling trade about the risks of infection and create
a reliable system for the safe removal and incineration of
needles before the syringes are put in the trash. If the recycling
of syringes for remoulded plastic cannot realistically be
stopped yet, at least the risks to everyone can be reduced.
In the short year since Pakistan
formed its national network for the Safe Injection Global
Network, no time has been wasted. Today, the network’s
activities are beginning to bear fruit: the country has recognized
the scale of its problem and – crucially – most
stakeholders in the health system are now keen to do something
about it.
References
(1)
Presentation at SIGN Pakistan symposium, February 2000, by
Dr Stephen Luby, CDC, Atlanta USA.
(2) Presentation
at SIGN Pakistan symposium, February 2000, by Dr Naheed Nabi,
Aga Khan University, Karachi, Pakistan.
(3) For an
update on current WHO policies and activities on healthcare
waste disposal, see http://www.who.int/inf-fs/en/fact253.html
and http://www.injectionsafety.org/documents/Aide-Memoire-HCWM.pdf
Phyllida Brown
|
|
Country file 2: Egypt: ‘We
need to decrease the demand for injections’
EGYPT knows better than most countries
the human cost of re-using needles. An astonishingly high
proportion of the population – about one in eight people
– is infected with hepatitis C virus (HCV), and hepatitis
B is also widespread(1). Much of this
disease burden is attributed to unsafe injections. The problem
is not new, but today there is a new and powerful commitment
to overcoming it.
"Injection safety and infection
control have become high priorities of the Ministry of Health
and Population," says Dr Maha Talaat, a public health specialist
and executive manager for a new programme in the ministry.
The programme’s goal is to prevent the transmission of
bloodborne pathogens in the health service. Dr Talaat is also
a member of a new national coalition of health workers that
is striving to increase awareness of injection safety issues.
Part of Egypt’s problem can
be traced back to a mass treatment for schistosomiasis before
the 1980s. The treatment required multiple injections and
is believed to have spread HCV widely(2).
But new cases of HCV infection have continued to appear today,
even though the schistosomiasis treatment has long been replaced.
Researchers believe that re-used needles are still to blame.
Today, studies suggest HCV continues to be spread by unsafe
injections and other healthcare practices.
Most of the injections are unnecessary.
"People prefer injections to oral medications because they
think that injections will cure them faster," says Dr Talaat.
"We need to decrease the demand for injections."
The government has planned its
response carefully. This year, the new programme is gathering
essential baseline data so that it can measure the impact
of interventions that will start next year, including training
for healthworkers, education and mass media campaigns for
the public, and action to ensure that supplies of sterile
injection equipment are available at all times.
The top priority, Dr Talaat believes,
is to educate those who deliver the injections. The first
step is to identify who they are. The team has already discovered,
from a study in one governorate, that more than 40% of injections
in this setting are given not by trained healthworkers but
by lay people including relatives, friends and "health barbers",
whose services are cheaper than those of doctors. These findings,
and further studies to find out healthworkers’ practices
across the country, will be crucial in the design and targeting
of training material.
Another key priority is safer
disposal systems for clinical waste, says Dr Talaat. "The
Ministry of Environmental Affairs, together with the Ministry
of Health and Population, are working to try to solve this
problem," says Dr Talaat. Because there is no proper system
for the transport and incineration of clinical waste, all
syringes – whether or not they are in safety boxes –
are a hazard once they leave the healthcare facility. Some
find their way to municipal rubbish dumps where children play
with them. If the final disposal system is not properly managed,
says Dr Talaat, no type of equipment, including safety boxes
or autodisable (AD) syringes, can be regarded as safe.
No one doubts the scale of the
challenge facing Egypt. But now it is recognized. And, with
a new government programme and an active coalition of healthworkers
determined to achieve change, the battle has begun.
References
(1)
WHO press release: http://www.who.int/inf-pr-2000/en/pr2000-14.html
(2) Frank
et al. The role of parenteral antischistosomal therapy
in the spread of hepatitis C virus in Egypt. The Lancet,
2000, 355: 887-891.
Phyllida Brown
|
Return to March 2001 contents
page
|